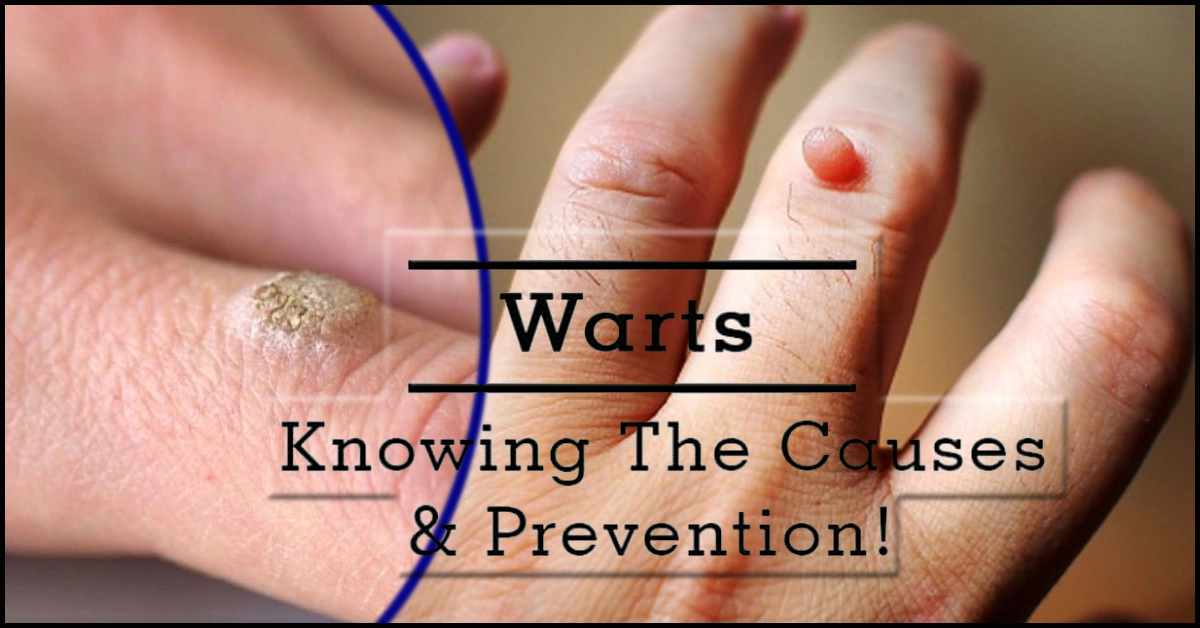
A Wart : Causes, Symptoms & Treatment Options
Wart : A Wart is a small, typically rough, and hard growth that appears on the skin or mucous membranes. It is caused by a viral infection, specifically by the human papillomavirus (HPV). Warts can occur on various parts of the body, such as the hands, feet, face, or genitals, depending on the type of HPV involved.
Warts are usually Non-cancerous and harmless, although they can be bothersome or unsightly. They can vary in appearance, ranging from flat and smooth to raised and cauliflower-like. Warts are contagious and can spread from person to person through direct contact or by touching surfaces contaminated with the virus.
Warts can often resolve on their own over time, as the immune system gradually eliminates the virus. However, some people may choose to treat warts for cosmetic reasons or if they cause discomfort or interfere with daily activities. Treatment options include over-the-counter medications (like salicylic acid), Cry Therapy (freezing), laser Therapy, surgical removal, or Immunotherapy. It’s important to consult with a Health care professional to determine the most appropriate treatment approach for your specific situation.
Causes and Transmission of Warts
The human papillomavirus (HPV) is the primary cause of warts. Here are the key points regarding the causes and transmission of warts:
1. Human Papillomavirus (HPV): Warts are primarily caused by specific strains of HPV. There are more than 100 known types of HPV, and each type tends to infect specific areas of the body.
2. Direct Contact: Warts are highly contagious and can be transmitted through direct skin-to-skin contact with an infected person. This can occur through activities such as shaking hands, touching, or sexual contact.
3. Indirect Contact: Warts can also spread indirectly through contact with objects or surfaces that have come into contact with an infected person’s wart. Sharing items like towels, razors, or shoes increases the risk of transmission.
4. Entry Points: HPV enters the body through tiny cuts, breaks, or abrasions in the skin. Areas of moist, damaged skin are particularly vulnerable to infection.
5. Risk Factors
Certain factors increase the likelihood of contracting and transmitting warts:
- Weakened immune system: People with Weakened immune systems, such as those with HIV/AIDS or Undergoing immunosuppressive Therapy, are more Susceptible to warts.
- Age: Warts are more common in children and young adults, possibly due to Increased Exposure and developing immune systems.
- Damaged skin: Any break in the skin, such as cuts, scrapes, or Hangnails, provides an entry point for the virus.
6. Persistence of the Virus: After Exposure to HPV, it may take weeks or even months for warts to develop. The virus can remain dormant in the body, making it possible for warts to appear long after initial Exposure.
It’s important to note that different types of HPV are responsible for various types of warts. While some strains cause common warts, others are linked to genital warts or certain cancers. Practicing good hygiene, Avoiding direct contact with warts, and taking Precautions to protect the skin can help reduce the risk of Contracting and Spreading warts.
Symptoms and Appearance of Warts
Warts have Distinctive Characteristics that can help identify them. Here are the key points regarding the symptoms and appearance of warts:
1. Small, Rough Growth: Warts Typically appear as small, raised growths on the skin or mucous membranes. They can range in size from a few Millimeters to a Centimeter or more in Diameter.
2. Texture: Warts often have a rough, Textured surface. The texture may Rsemble a Cauliflower or have Irregular, bumpy Projections.
3. Color
Warts can vary in color, depending on the type and location:
- Common Warts: Common warts are often grayish-brown or flesh-colored.
- Plantar Warts: Plantar warts on the soles of the feet may have a calloused or thickened skin covering, making them appear yellowish or gray.
4. Different Shapes and Locations: Warts can have various shapes and appear on different parts of the body, including:
- Round or irregular shape: Common warts and plantar warts often have a rounded or irregular shape.
- Flat, Smooth Appearance: Flat warts have a smooth, flat surface and can occur in large numbers, often on the face, hands, or legs.
- Filiform Warts: Filiform warts have thread-like projections and commonly appear on the face, particularly around the mouth or nose.
- Genital Warts: Genital warts can be flat or raised and have a cauliflower-like appearance. They primarily affect the genital and anal areas.
5. Clusters or Singular Growth: Warts can occur individually or in clusters, especially in the case of flat warts and genital warts.
6. Pain or Discomfort: In most cases, warts do not cause pain or discomfort. However, certain types of warts, such as plantar warts on weight-bearing areas, can cause pain or tenderness when walking or standing.
It’s important to note that warts can vary in appearance, and their characteristics may depend on factors such as the specific type of HPV involved, the location of the wart, and individual variations. If you suspect you have a Wart or are unsure about any skin growth, it’s recommended to consult a Health care professional for an accurate diagnosis.
Also Read – Thyroid Disorders: Understanding, Diagnosis, Treatment, and Support
Treatment Options for Wart
There are several treatment options available for warts, depending on the type, location, and severity of the warts. Here are the key treatment options:
1. Over-the-Counter Medications:
- Non-prescription Wart treatments usually contain Ingredients like Salicylic acid or lactic acid.
- These medications are available in various forms, such as liquids, gels, Ointments, or Medicated pads.
- They operate by chipping away at the Wart over time in layers. Regular application and following the instructions are important for Effectiveness.
2. Cry Therapy:
- Cry Therapy Involves freezing the Wart with liquid Nitrogen or other freezing agents.
- The freezing process destroys the Wart tissue, causing it to slough off over time.
- Cry Therapy is Typically Performed by a Health care professional and may require multiple sessions for complete Wart removal.
3. Laser Therapy:
- Laser Therapy uses a focused laser beam to destroy the Wart tissue.
- The laser heats and destroys the blood vessels that supply the wart, leading to its removal.
- Laser Therapy is usually Performed by a Dermatologist and may require multiple sessions.
4. Surgical Removal:
- Surgical removal involves cutting out the Wart using a scalpel or other Surgical tools.
- Local anesthesia is Frequently used during this surgery.
- Surgical removal is commonly used for large or Resistant warts or when other treatments have not been effective.
5. Immunotherapy:
- Immunotherapy aims to Stimulate the immune system to recognize and attack the wart.
- This treatment option is usually Reserved for stubborn or Recurrent warts.
- Immunotherapy can involve Injecting Substances such as candida antigen or Interferon into the Wart or Applying Immune-stimulating creams or solutions.
It’s important to consult with a Health care professional, such as a Dermatologist, to determine the most appropriate treatment option for your specific situation. They can assess the type, location, and Severity of the warts and recommend the best course of action. Self-treatment is not always Advisable, especially for warts on sensitive areas or in Individuals with certain medical conditions.
Prevention and Precautions for Wart
Taking Preventive measures and Practicing Precautions can help reduce the risk of contracting and spreading warts. Here are some important Prevention Strategies:
1. Good Hygiene:
- Wash your hands regularly with soap and water to Minimize the spread of HPV and other infections.
- Avoid touching warts on yourself or others to prevent the spread of the virus.
2. Avoid Direct Contact:
- Direct Skin-to-skin contact should be avoided while around people who have visible warts.
- Refrain from sharing personal items such as towels, razors, or shoes, especially if the other person has warts.
3. Protect Skin:
- Keep skin clean and dry to reduce the risk of Developing warts on areas prone to Moisture.
- Avoid walking Barefoot in public areas such as swimming pools, locker rooms, and Communal showers where HPV may be present.
4. Wear Protective Footwear:
- When using public showers or walking in Communal areas where HPV may be present, wear Waterproof sandals or Flip-flops to Minimize the risk of Contracting plantar warts.
5. Boost Immune System:
- Maintain a Health y Lifestyle with a Balanced diet, regular exercise, and Adequate sleep to support a strong immune system.
- Certain Lifestyle factors, such as stress, poor Nutrition, and lack of sleep, can weaken the immune system and make Individuals more Susceptible to infections.
6. HPV Vaccination:
- Consider getting Vaccinated against HPV to reduce the risk of Developing certain types of warts, including genital warts.
- The HPV vaccine is Typically Recommended for both males and females in their early teenage years, but it can also be Administered up to certain ages in both genders.
7. Prompt Treatment:
- If you develop a wart, seek prompt medical attention and follow the recommended treatment options to prevent further spread and recurrence.
Remember, while preventive measures can reduce the risk of contracting warts, they do not guarantee complete protection. It’s important to maintain good overall hygiene practices and consult with a Health care professional for personalized advice and guidance based on your specific circumstances.
Risk Factors for Wart
Several factors can increase an individual’s susceptibility to warts. Understanding these risk factors can help identify those who may be more prone to developing warts. Here are the key risk factors associated with warts:
- Age: Warts are more common in children and young adults, with the highest incidence occurring in Individuals under the age of 30. This may be due to increased exposure to the virus and a developing immune system.
- Weakened Immune System: Individuals with weakened immune systems are at a higher risk of developing warts. Conditions such as HIV/AIDS, organ transplantation, and certain medications that suppress the immune system can increase susceptibility.
- Skin-to-Skin Contact: Direct skin-to-skin contact with an infected person or touching surfaces contaminated with the virus increases the risk of contracting warts. This is particularly relevant in environments where people share close quarters, such as schools, gyms, and communal living spaces.
- Damaged Skin: Warts often develop in areas where the skin is damaged, such as cuts, scrapes, or hangnails. Openings in the skin provide an entry point for the HPV virus, increasing the likelihood of infection.
- Occupation or Activities: Certain occupations or activities that involve frequent contact with contaminated surfaces or exposure to moist environments may increase the risk of developing warts. Examples include Health care workers, swimmers, and Individuals involved in occupations that require prolonged glove use.
- Personal or Sexual Contact: Engaging in sexual activity with an infected individual can lead to the transmission of genital warts, which are caused by specific strains of HPV. The risk is higher in Individuals who have multiple sexual partners or engage in unprotected sex.
- Previous History of Warts: Individuals who have had warts in the past are more likely to develop new warts in the future. This suggests a higher susceptibility to the virus.
Complications of Wart
While warts are generally harmless and benign, they can sometimes lead to certain complications. Here are some potential complications associated with warts:
- Spread to other areas: Warts can spread to nearby skin through self-inoculation. Scratching or picking at a Wart and then touching another part of the body can cause the virus to transfer, leading to the development of new warts in different locations.
- Secondary Infections: Warts can create openings in the skin, making it susceptible to bacterial infections. Scratching or picking at warts can introduce bacteria, leading to redness, swelling, pain, and discharge. Prompt medical attention is required if signs of infection develop.
- Psychological Impact: Visible warts, especially in noticeable or sensitive areas, can cause emotional distress and impact an individual’s self-esteem and body image. This is particularly relevant for genital warts, which may contribute to anxiety, embarrassment, or changes in sexual behavior.
- Recurrence: Warts can sometimes recur even after successful treatment. This may be due to the persistence of HPV in the body or reinfection from the environment. Proper preventive measures and follow-up care are important to reduce the risk of recurrence.
- Malignant Transformation (Rare): While rare, certain types of HPV that cause genital warts, such as high-risk strains, have the potential to cause cellular changes and increase the risk of developing certain types of cancer, including cervical, anal, or penile cancer. Regular screening and appropriate medical management are essential for early detection and treatment of any concerning changes.
It’s important to note that complications from warts are relatively uncommon, and most warts can be successfully treated or managed. Seeking timely medical advice, following recommended treatment options, practicing good hygiene, and taking preventive measures can help minimize the risk of complications associated with warts.
Home Remedies and Precautions for Wart
While medical treatments are often recommended for warts, there are some home remedies and precautions that may help in managing warts or reducing their symptoms. It’s important to note that home remedies may not work for everyone, and it’s advisable to consult a Health care professional for proper diagnosis and guidance. Here are some common home remedies and precautions for warts:
1. Salicylic Acid:
- Over-the-counter Wart treatments containing Salicylic acid are commonly used at home.
- Follow the instructions carefully and apply the product directly to the Wart to Gradually remove it.
- Before applying the medication, soak the Wart in warm water to soften it for better Absorption.
2. Duct Tape Occlusion:
- Covering the Wart with duct tape may help to suffocate the Wart and stimulate the immune system.
- Clean the area, apply the duct tape, and leave it on for about six days. Then, remove the tape, soak the Wart in warm water, and gently file the Wart with a pumice stone or emery board.
- Repeat the process until the Wart disappears.
3. Garlic:
- Garlic has antimicrobial properties and may help in managing warts.
- Apply the juice from a crushed garlic clove immediately on the wart. Cover it with a bandage or duct tape overnight.
- Repeat daily until the Wart diminishes.
4. Tea Tree Oil:
- Tea tree oil has antiviral and antiseptic properties that may assist in Wart treatment.
- Dilute tea tree oil with a carrier oil (such as coconut oil) and apply it to the wart.
- Apply duct tape or bandage to the Wart. Repeat daily until the Wart improves.
5. Good Hygiene Practices:
- Maintain proper hygiene to stop the spread of warts.
- Wash your hands regularly with soap and water, especially after touching warts or affected areas.
- Avoid picking or scratching warts to minimize the risk of spreading the virus.
6. Avoid Sharing Personal Items:
- Refrain from sharing personal items like towels, razors, or shoes to minimize the risk of spreading the virus to others or developing new warts.
It’s important to monitor the progress of home remedies and consult a Health care professional if the warts persist, worsen, or cause discomfort. Professional medical treatments may still be necessary in some cases.
Recurrence of Wart
Warts have the potential to recur even after successful treatment. The recurrence of warts can be attributed to several factors, including:
- Persistence of HPV: Warts are caused by the human papillomavirus (HPV), which can remain dormant in the body even after visible warts have been treated or resolved. The virus can reactivate, leading to the development of new warts in the same or different areas.
- Reinfection: After successful treatment, Individuals can be reinfected with HPV if they come into contact with the virus again. This can occur through skin-to-skin contact with an infected person or by touching surfaces contaminated with the virus.
- Incomplete Treatment: If warts are not fully treated or removed, residual virus or Wart tissue may remain. This can increase the likelihood of regrowth or recurrence.
- Weakened Immune System: A weakened immune system can make Individuals more susceptible to recurrent warts. Conditions such as stress, illness, certain medications, or immune system disorders can impair the body’s ability to fight off HPV effectively.
- Subclinical Infection: Subclinical infections refer to the presence of HPV without any visible signs of warts. These infections can be challenging to detect, and Individuals with subclinical infections may unknowingly spread the virus or develop visible warts later on.
To minimize the risk of recurrent wart
it is important to take the following precautions:
- Follow Treatment Instructions: When receiving professional medical treatment for warts, ensure that you follow the recommended treatment plan and complete the entire course of treatment. This helps to ensure the complete elimination of the Wart and the virus.
- Boost Immune System: Maintain a Health y lifestyle, including a balanced diet, regular exercise, adequate sleep, and stress management, to support a strong immune system. A robust immune system can help prevent the reactivation of HPV and reduce the risk of recurrent warts.
- Practice Good Hygiene: Adhere to good hygiene practices, such as regular handwashing with soap and water, especially after touching warts or affected areas. Avoid picking or scratching warts, as it can lead to spreading the virus or triggering the recurrence of warts.
- Monitor for Early Signs: Stay vigilant and monitor the skin for any early signs of warts. Promptly seek medical attention if you notice any new growths or changes in existing warts.
It’s important to consult with a Health care professional for an accurate diagnosis, appropriate treatment, and guidance on preventive measures to minimize the risk of recurrent warts.
Also Read – Hair Loss: Causes, Prevention, and Treatment
HPV Vaccination
HPV vaccination is an effective preventive measure against certain types of the human papillomavirus (HPV) that can cause various diseases, including genital warts and certain types of cancers. Here are some key points about HPV vaccination:
- Purpose: HPV vaccines are designed to protect against infection with specific types of HPV that are known to be associated with genital warts and cancers, such as cervical, anal, vulvar, vaginal, penile, and oropharyngeal (throat) cancers.
- Target Age Group: HPV vaccination is typically recommended for adolescents and young adults, starting between the ages of 9 and 12. Vaccination at an early age ensures protection before potential exposure to HPV through sexual activity.
- Vaccine Types: There are several HPV vaccines available, including the bivalent, quadrivalent, and nonvalent vaccines. These vaccines provide protection against different types of HPV. The specific vaccine type and dosing schedule may vary based on factors such as age, sex, and country-specific guidelines.
- Effectiveness: HPV vaccines have been shown to be highly effective in preventing HPV infections and associated diseases. They offer protection against the specific HPV types included in the vaccine. However, the vaccines do not protect against all types of HPV, so it is still important to practice safe sexual behaviors and undergo regular screenings as recommended by Health care professionals.
- Safety: HPV vaccines have undergone extensive testing and have been found to be safe. Common side effects are typically mild and include pain, redness, or swelling at the injection site. Serious side effects are rare. As with any vaccine, it is essential to discuss any specific concerns or medical conditions with a Health care professional before receiving the vaccination.
It is important to consult with a Health care professional to determine the suitability of HPV vaccination based on individual circumstances, including age, sex, and Health status.
Genital Wart
Condylomas acuminate, generally referred to as genital warts, are a STI brought on by certain strains of the human papillomavirus (HPV). Here’s some important information about genital warts:
1. Transmission: Genital warts are primarily transmitted through sexual contact, including vaginal, anal, or oral sex. They can be spread even if the infected person does not have visible warts. The virus can also be transmitted through non-penetrative sexual activities involving skin-to-skin contact.
2. Symptoms: Genital warts usually appear as small, flesh-colored or gray growths in the genital or anal area. They can vary in size and shape, and may appear as single warts or in clusters. In some cases, they may be flat or barely visible. Genital warts can cause itching, discomfort, and, rarely, bleeding.
3. HPV Types: Genital warts are primarily caused by certain strains of HPV, particularly types 6 and 11. These types of HPV do not typically cause cancer. However, it’s important to note that other high-risk types of HPV can cause cervical, anal, and other types of cancer.
4. Diagnosis: A Health care professional can diagnose genital warts through a visual examination of the affected area. In some cases, a biopsy may be performed to confirm the diagnosis or rule out other conditions. Additionally, Individuals with genital warts may be advised to undergo further testing for other sexually transmitted infections.
5. Treatment: There is no cure for HPV, but treatment options are available to manage and remove visible genital warts. These may include topical medications applied directly to the warts, Cry Therapy (freezing the warts with liquid nitrogen), electrocautery (burning the warts), surgical removal, or laser Therapy. Treatment aims to remove visible warts, alleviate symptoms, and reduce the risk of transmission.
6. Prevention
Preventive measures can reduce the risk of contracting and spreading genital warts:
- HPV Vaccination: HPV vaccines are available and recommended for both males and females to prevent HPV infections, including those that cause genital warts.
- Safe Sexual Practices: Practicing safe sex, including consistent and correct condom use, can reduce the risk of HPV transmission. However, since HPV can infect areas not covered by condoms, complete protection is not guaranteed.
- Regular Screening: Regular cervical cancer screenings for Individuals with a cervix, such as Pap tests or HPV tests, are important for early detection of cervical abnormalities or cancer.
It’s important to consult with a Health care professional for proper diagnosis, treatment, and guidance related to genital warts. They can provide personalized recommendations based on individual circumstances and help address any concerns or questions.
Diagnosis of Genital Wart
The diagnosis of genital warts typically involves a combination of a physical examination and, in some cases, additional tests. Here’s an overview of the diagnostic process for genital warts:
- Physical Examination: A Health care professional, such as a dermatologist or gynecologist, will conduct a visual inspection of the affected area. They will look for the characteristic signs of genital warts, including the appearance of small, flesh-colored or gray growths in the genital or anal area. The Health care professional may use a magnifying instrument, such as a colposcope, to examine the warts more closely.
- Medical History: The Health care professional will inquire about your medical history and sexual activity to assess the likelihood of genital warts and potential risk factors for other sexually transmitted infections (STIs).
- Biopsy (if necessary): In some cases, a biopsy may be recommended to confirm the diagnosis or rule out other conditions. During a biopsy, a small sample of tissue from the Wart or affected area is taken for laboratory analysis. This procedure is typically performed if the diagnosis is uncertain or if there are atypical features present.
- Additional Testing: Depending on the circumstances, additional testing may be performed to screen for other sexually transmitted infections. For example, Individuals with genital warts may be advised to undergo testing for high-risk strains of HPV or for other common STIs, such as chlamydia or gonorrhea.
It’s advisable to consult with a Health care professional, such as a dermatologist, gynecologist, or primary care provider, for an accurate diagnosis and appropriate management of genital warts. They can provide personalized recommendations, discuss treatment options, and address any questions or concerns you may have.
Psychological Impact
The presence of genital warts can have a psychological impact on individuals. Here are some key points to consider regarding the psychological aspects of genital warts:
- Emotional Distress: Being diagnosed with genital warts can cause emotional distress, including feelings of embarrassment, shame, anxiety, and sadness. The visible nature of the warts and their association with sexual activity may lead to concerns about body image, self-esteem, and intimate relationships.
- Stigma and Social Impact: Genital warts are often stigmatized due to their connection to sexually transmitted infections. This stigma can lead to feelings of isolation, fear of judgment or rejection from partners, and difficulty discussing the condition with friends, family, or Health care providers.
- Impact on Sexual Well-being: Genital warts can affect an individual’s sexual well-being. Concerns about transmitting the infection to a partner, discomfort or pain during sexual activity, or reduced sexual desire may arise. It is important to communicate openly and honestly with sexual partners about the presence of genital warts and to practice safe sex to minimize the risk of transmission.
- Relationship Challenges: Genital warts can impact relationships, particularly if there is a lack of understanding or miscommunication about the condition. Partners may experience concerns about their own Health , potential transmission, or trust issues. Open and supportive communication is crucial for navigating these challenges together.
- Education and Awareness: Increasing awareness and knowledge about genital warts can help reduce stigma and improve understanding. Education about the causes, transmission, treatment options, and preventive measures can empower Individuals to make informed decisions and alleviate anxiety or misconceptions.
It is important to remember that genital warts are a common condition, and many Individuals have successfully managed and overcome the psychological impact associated with them. Seeking support from Health care professionals, partners, friends, or support groups can provide valuable emotional assistance during this time.
Professional Treatment Considerations
When it comes to professional treatment for genital warts, there are several considerations to keep in mind. Consider the following significant factors:
- Consultation with a Health care Professional: If you suspect or have been diagnosed with genital warts, it is essential to consult with a Health care professional, such as a dermatologist, gynecologist, or primary care provider. They have the expertise to accurately diagnose and recommend appropriate treatment options based on your individual circumstances.
- Treatment Options: Health care professionals can discuss various treatment options available for genital warts. These may include topical medications, such as creams or solutions applied directly to the warts, Cry Therapy (freezing the warts with liquid nitrogen), electrocautery (burning the warts), surgical removal, or laser Therapy. The selection of a course of therapy is influenced by personal preferences as well as elements including the size, location, and number of warts.
- Expertise and Experience: Health care professionals who specialize in dermatology or gynecology have experience in managing genital warts. They are familiar with the latest treatment guidelines, have access to advanced treatment modalities, and can provide personalized care based on your specific needs.
- Monitoring and Follow-up: After initiating treatment, it is important to follow up with your Health care professional as scheduled. They can assess the response to treatment, monitor for any adverse effects, and provide guidance on ongoing care. Regular follow-up visits also allow for the early detection of any recurrent or new warts that may require further intervention.
- Comprehensive Sexual Health Evaluation: In addition to addressing the visible warts, Health care professionals may recommend a comprehensive sexual Health evaluation. This may include screening for other sexually transmitted infections, discussing safe sex practices, and providing education on HPV vaccination for eligible individuals.
Remember that each individual’s situation is unique, and treatment recommendations may vary.
Summary
The human papillomavirus (HPV) is a sexually transmitted infection that can result in genital warts. They appear as small, flesh-colored or gray growths in the genital or anal area and can cause discomfort and itching. Genital warts are primarily transmitted through sexual contact, and their diagnosis involves a physical examination by a Health care professional.
Treatment options for genital warts include topical medications, Cry Therapy , electrocautery, surgical removal, or laser Therapy. There is no cure for HPV, but these treatments aim to remove visible warts, alleviate symptoms, and reduce the risk of transmission. It is important to consult with a Health care professional for an accurate diagnosis and appropriate treatment recommendation.
Genital warts can have a psychological impact on individuals, leading to emotional distress, concerns about body image, and challenges in relationships. Seeking psychological support and education about the condition can help manage these effects. Health care professionals can provide referrals to support services and offer guidance on preventive measures, such as safe sex practices and HPV vaccination.
Professional treatment considerations involve consulting with Health care professionals experienced in managing genital warts, exploring treatment options, and following up for monitoring and evaluation. They can also provide comprehensive sexual Health evaluations and address the emotional aspects of genital warts. Maintaining open communication and active involvement in treatment decisions is crucial for personalized care.
Remember that genital warts are a common condition, and with appropriate treatment and support, Individuals can effectively manage the infection and its impact on their lives.
Disclaimer:
The information on this website is provided for Informational reasons and is not meant to be personal medical advice. You should consult your doctor or another Qualified fitness professional if you have any concerns about a Systemic condition. Never Disregard professional medical advice or give up looking for it because of something you read on this website. The Daddydontblog.com does not promote or recommend any products.





Hello everyone i am here to testify and enlighten you on how you can be cured from the disease/virus known as Herpes, as the FDA described that it cannot be cured or there is no cure for it, not knowing that natural herbal treatment is highly recommended for the treatment and cure for Herpes its easy and it has no side effect, are you interested in curing herpes now, I am a living testimony of how Dr Ogedegbe cured me with natural herbs which I bought from him. You can cure your Diabetes, Hiv, Hepatitis a, b, Gonorrhea, Fibroids ,Infertility ,Epilepsy, Syphilis, Chronic infection, Copd, ,Std, Cancer, Hpv Hsv1&2, ED, Penis enlargement, Weak erection .etc……… for more info send him a DM on….. WhatsApp +2348109374702 or Email dr.ogedegbe6@gmail.com